All articles
Healthcare Sector Moves to Bring Patient Experience Up to Modern Consumer Standards
Sven Gierlinger, Chief Experience Officer at Northwell Health, outlines how unifying human, digital, and physical touchpoints can reduce friction in care.

Key Points
When the human, digital, and physical parts of care fail to work together, the patient journey often breaks down, creating friction for today’s consumers.
Sven Gierlinger, Chief Experience Officer at Northwell Health, explains how his hospitality background shapes a unified model for modern patient experience.
He shows how improvements to food, space, and digital tools like ambient listening create a seamless journey that restores connection and reduces administrative strain.
I look at it as a Venn diagram with three circles: the human experience, the digital experience, and the physical experience, all overlapping with the patient in the center.
The modern healthcare experience is no longer just about bedside manner. Now, it lives or dies by how well the people, the technology, and the spaces around a patient work together. When those pieces move out of sync, the whole system is plagued by friction. It's especially jarring for consumers who have grown used to faster, simpler, more intuitive service in every other part of their lives.
Sven Gierlinger, Chief Experience Officer at Northwell Health, knows this friction better than most. Having spent nearly two decades in hospitality before moving into healthcare, with nearly a decade at The Ritz-Carlton, Gierlinger has carried that hospitality instinct with him ever since. Today, his approach treats the patient journey as a complete sensory experience rather than a series of clinical tasks—one he anchors in a single, simple framework.
"I look at it as a Venn diagram with three circles: the human experience, the digital experience, and the physical experience, all overlapping with the patient in the center. All three are important aspects of the totality of the experience, and they have to be in harmony to work together," Gierlinger says. For him, a warm greeting, a modern space, and a seamless digital process should feel like one continuous patient experience rather than three separate touch points.
Prime standard: Now accustomed to on-demand service in every other part of life, the healthcare consumer brings those expectations into their care experience. The disconnect is a growing liability, Gierlinger explains, and failing to close that gap is becoming a strategic risk. "If Amazon can get you a package you ordered to your door in four hours, why does it take two months to get an appointment in healthcare?"
The weight of waiting: But fixing the problem also means addressing the institutional mindset that overlooks the non-clinical parts of the experience first. Here, Gierlinger compares the healthcare system with the hospitality industry's obsession with service, in which the goal is to "move heaven and earth" to solve a problem. "The old attitude was that a waiting list was good enough. That mindset is shifting, because patients now have the power and the choice to go where they want. If they don't get what they need from us, they will go somewhere else."
Gierlinger’s strategy for harmonization begins by applying lessons from the hotel industry, which designs spaces to "enliven the senses and instill well-being." Pointing to hospital-provided food as an often-overlooked part of the patient experience, he describes it as the perfect "low-hanging fruit" to prove his point.
It's not brain surgery: An initiative to overhaul Northwell’s food program began with a former Plaza Hotel chef and has since grown into a culinary team that now includes a Michelin-starred team. Describing it as "an overlooked opportunity," Gierlinger explains how, "it turns out that actually serving delicious food that is fresh and tastes good is not that hard to do. It's a lot easier to do than getting brain surgery right, but healthcare has just not focused on it."
Out of body experience: But the impact has been unmistakable. "Patients tell us they get so absorbed in the menu that they actually forget they were in pain," Gierlinger says. "We hear that the experience transports them out of the hospital, making them feel like they're in a restaurant." In his opinion, the food program demonstrates that improving a single non-clinical touchpoint can strengthen, and even elevate, the value of clinical care itself. Meanwhile, the change is reflected directly in outcomes as Northwell’s food quality scores climbed from the ninth to the 90th percentile.
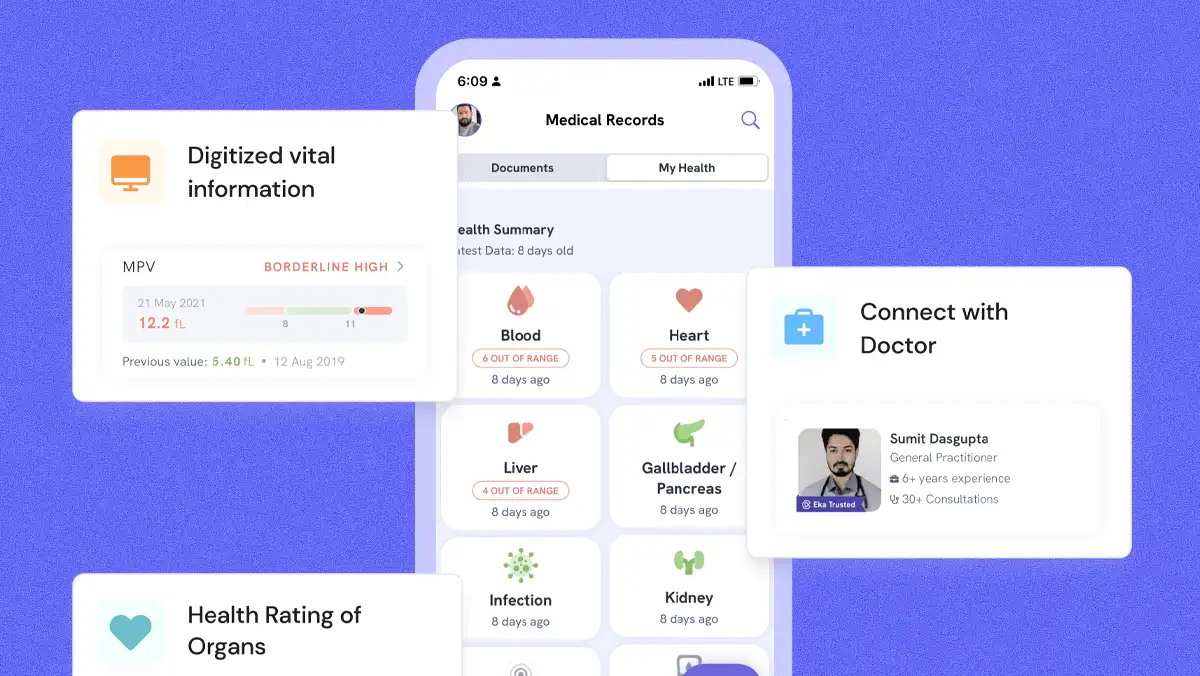
With the physical experience addressed, the framework shifts to the digital circle. Gierlinger draws a clear line between the clinical journey and the administrative one that covers billing, appointments, and test results. While clinical care has steadily improved, the administrative experience has been left behind—even though it defines much of how patients judge their care.
Banking on CX: Other high-stakes industries have already made the shift, Gierlinger says. "People worry about two things: their financial health and their physical health," he said. "If we can do all our banking on a phone, we can do it in healthcare." But it's really not that complicated, he adds. "The ideal digital experience is one where I've already registered and paid my co-pay before I even arrive. I show up and don't get handed a clipboard with the same information I’ve filled out a dozen times."
Eye to eye: The framework achieves its full potential when the digital circle works in harmony with the human one, Gierlinger says. Pointing to AI as a key part of the solution to the supposed tech-vs-warmth paradox, he sees technology as a way to restore humanity to healthcare encounters that are often cold and clinical. "If technology is used well, it will actually amplify the human experience. Ambient listening is a great example of that."
The benefit is immediately evident at the bedside. "It takes the burden away from the clinician of being tethered to a keyboard," Gierlinger says. "They can just have that clinical encounter, look the patient in the eye, and talk to them. The technology creates the clinical notes and the follow-up, and they just approve it, which saves a lot of time."
In the end, Gierlinger's framework isn’t about any single app or initiative. It’s a philosophy that requires total organizational commitment to viewing the patient journey as a single, unified whole and to making tangible investments in modern facilities and core enterprise technologies. For him, orchestrating this harmony depends on one essential factor above all others: leadership. "It takes leadership commitment, coordination, and collaboration to make sure that this all works well together."